Healthcare Reform in 2013 and Beyond
The recent ruling on the Patient Protection and Affordable Care Act (PPACA) by the U.S. Supreme Court has given employers much to consider for the future of their sponsored healthcare plans.
The recent ruling on the Patient Protection and Affordable Care Act (PPACA) by the U.S. Supreme Court has given employers much to consider for the future of their sponsored healthcare plans. The good news is that employers have another 12-plus months to map out their strategies relative to the “pay or play” mandate (and corresponding tax/penalties) and the forthcoming healthcare exchanges. However, there are healthcare reform issues that employers should be aware of for 2013. These include: $2,500 salary reduction limitation on health flexible spending accounts (FSAs) under a cafeteria plan; the requirement to distribute and make available Summaries of Benefits and Coverage (SBCs); covering women’s preventive health services at 100 percent; and, reporting the value of the health plan on Form W-2.
Beginning with plan years after December 31, 2012, there is a contribution limit of $2,500 on health FSAs. This new limitation may require you, as an employer, to revise your Section 125 plan document and communicate this to employees. IRS Notice 2012-40 clarified that this limitation would be effective based on plan year rather than taxable year.
SBCs must be provided or made available to all applicants and participants in the employer-sponsored health plan beginning with the first open enrollment on or after Sept. 23, 2012. This is mostly an administrative task; however, there are specific differences with the responsible party depending upon whether the plan is fully insured or self-insured. Furthermore, there are a number of specific details regarding how the SBC must be distributed. Lastly, employers will need to consider how the SBC requirements are met relative to carve-out prescription drug plans, health reimbursement arrangements (HRAs),etc. It should be noted that the SBC requirement cannot be met simply by distributing existing benefit summaries or summary plan descriptions. In addition to the language used, the SBC must be drafted using a specific number of pages, spacing and font requirements. Examples and templates can be found on the Department of Labor’s website (dol.gov).
For fully-insured plans the insurance company has the responsibility for compliance. For self-insured plans, it is the plan sponsor (the employer). For those employers that have both plans, it falls to both carrier and plan sponsor/employer. This is especially complex for those employers that have adopted HRAs or “wrap plans” because there are actually two plans: one fully insured and one self-insured. The self-insured plan is the HRA or “wrap,” and the fully-insured plan is the underlying medical plan. Each requires an SBC.
We recommend employers begin considering the impacts of the 2014 changes now: the number of full-time equivalents employed; penalties that might apply; net cost impact of the penalties; compensation adjustments for the potential to eliminate employer-sponsored benefits; the net cost impact of any compensation adjustments; from an employee’s perspective, the net buying power of a compensation adjustment; the recruiting/retention impact of any benefit and compensation changes; and whether or not the healthcare exchanges are accessible for the employer.
It’s likely that healthcare reform is going to impact each employer differently in 2014. Things such as average family income and part-time vs. full-time employee counts will influence the strategies considered. While healthcare reform has changed the landscape of employer-sponsored health plans significantly, one thing has not changed: a single solution applicable to all employers simply does not exist.
For More Information:
Plante Moran
(248)37507281/scott.mclellan@plantemoran.com
(248) 375-7412/ed.murphy@plantemoran.com
(248) 375-7475/jonathon.trionfi@plantemoran.com
plantemoran.com
Related Content
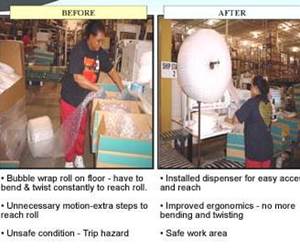
Making Quick and Easy Kaizen Work for Your Shop
Within each person is unlimited creative potential to improve shop operations.
Read MoreMMT Chats: Marketing’s Impact on Mold Manufacturing
Kelly Kasner, Director of Sales and Marketing for Michiana Global Mold (MGM) talks about the benefits her marketing and advertising, MGM’s China partnership and the next-generation skills gap. This episode is brought to you by ISCAR with New Ideas for Machining Intelligently.
Read MoreFrom Injection Mold Venting to Runnerless Micro Molds: MMT's Top-Viewed June Content
The MoldMaking Technology team has compiled a list of the top-viewed June content based on analytics. This month, we covered an array of topics including injection mold venting, business strategies and runnerless micro molds. Take a look at what you might have missed!
Read MoreHow to Improve Your Current Efficiency Rate
An alternative approach to taking on more EDM-intensive work when technology and personnel investment is not an option.
Read MoreRead Next
Reasons to Use Fiber Lasers for Mold Cleaning
Fiber lasers offer a simplicity, speed, control and portability, minimizing mold cleaning risks.
Read MoreHow to Use Strategic Planning Tools, Data to Manage the Human Side of Business
Q&A with Marion Wells, MMT EAB member and founder of Human Asset Management.
Read More



.jpg;maxWidth=300;quality=90)

_300x250 3.png;maxWidth=300;quality=90)